A Sea Change in the Recognition of Chronic Lyme Disease
The critical impact of a groundbreaking new study adds to the growing acknowledgement of this overlooked chronic disease.
The medical community has long struggled with diagnosing and recognizing certain chronic conditions. Diseases like lupus, long COVID, and Gulf War Syndrome were initially met with skepticism; in some cases it took years of research and advocacy to gain recognition and develop effective treatment options.
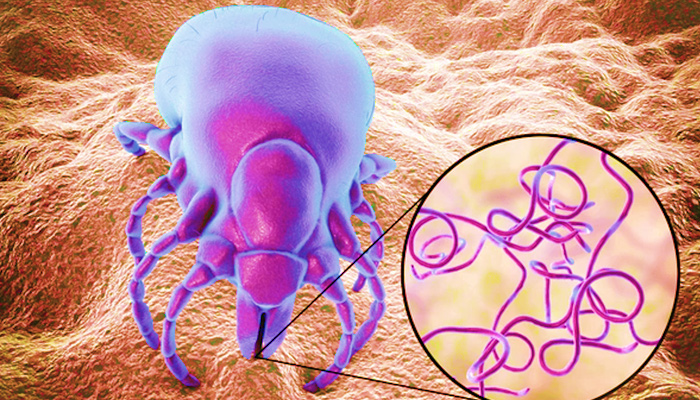
Chronic Lyme disease, also known as Post-Treatment Lyme Disease Syndrome (PTLDS), has faced similar challenges. Patients and advocates have long fought for recognition from the broader medical community and policymakers. Despite evidence of persistent symptoms in a significant percentage of Lyme disease patients, those suffering from chronic Lyme have often been dismissed, been prescribed yet another round of antibiotics or told their symptoms are psychosomatic. The battle for recognition has been a source of frustration and alienation for both patients and the medical professionals who support them.
NASEM’s Recent Move to Study Chronic Lyme Disease
In a significant reversal of policy, the National Academies of Sciences, Engineering, and Medicine (NASEM) has launched a comprehensive study to evaluate the evidence base for Lyme infection-associated chronic illnesses, including chronic Lyme disease. NASEM’s study aims to address existing research gaps, improve diagnostic criteria and develop standardized treatment protocols. The study, expected to be completed by early 2025, has the potential to shift the medical community’s approach to chronic Lyme disease and influence future policies [1].
The rapid spread of Lyme disease, primarily through infected deer ticks, has led to a significant increase in chronic Lyme sufferers, presenting severe challenges for those affected. Patients often endure persistent symptoms like severe fatigue, joint and muscle pain, cognitive difficulties and neurological issues. These symptoms result in substantial emotional distress, as patients struggle to find validation and effective treatment. The economic impact is equally profound, with ongoing medical expenses and lost productivity imposing a heavy burden on individuals and their families.
Our healthcare system bears the burden as well; according to a CDC report, the estimated economic burden of self-reported chronic Lyme disease in the United States—including direct medical costs and lost productivity—ranges from approximately $712 million to over $1.3 billion annually, underscoring the urgent need for effective interventions [2].
The Resistance of Established Medical Organizations
The battle for recognition of chronic Lyme disease has also created deep divisions within the medical community. Patients often report being dismissed by healthcare providers, who suggest that their symptoms are “all in their head.” This dismissal not only exacerbates their suffering but also leads to a breakdown in trust between patients and the medical system. On the other hand, medical professionals who advocate for chronic Lyme patients or explore alternative treatments often face professional ostracization.
Some clinicians like Dr. Charles Ray Jones, known for his controversial treatment of children with chronic Lyme disease, have been labeled as “Lyme-literate” doctors—a term that carries a stigma within mainstream medical circles. The fact that being “literate” in a disease bears a negative connotation and speaks volumes.
Advocacy groups have documented numerous cases where doctors have faced sanctions or professional backlash for their efforts to help chronic Lyme patients, deepening the divide between patients and mainstream medicine [3].
Doctors, policy makers and established medical organizations have been reluctant to embrace chronic Lyme disease as a legitimate condition due to several concerns. One primary issue has been the reliability of diagnostic tests. Current tests for Lyme disease, particularly for chronic cases, have been criticized for their lack of sensitivity and specificity.
The most widely used test, the Western Blot, can produce a substantial number of false-positive results, particularly in low-risk settings. For instance, an analysis published in the Journal of Infectious Diseases indicated that even with positive ELISA tests, the Western blot’s posttest probability for confirming Lyme disease may be as low as 4% to 10% in certain scenarios (Oxford Academic).
If the Western Blot has problems with specificity, current chronic Lyme tests have significant problems with sensitivity. “The serological tests commonly used to diagnose Lyme disease may not detect the disease in its later stages, leading to false negatives,” according to the Infectious Diseases Society of America (IDSA) [3]. This uncertainty has fueled skepticism about the validity of chronic Lyme as a diagnosis.
Diagnostic uncertainty leads to undertreatment; in most cases the use of long-term antibiotic therapy—often advocated by chronic Lyme disease supporters—has been discouraged due to concerns about antibiotic resistance and potential harm. Studies cited by the CDC have shown that despite support by Lyme advocates, prolonged antibiotic treatment has not consistently demonstrated clear benefits for chronic Lyme patients and may carry significant risks, including the development of antibiotic-resistant bacteria and adverse side effects [2].
Re-evaluating Assumptions
Recent developments have now begun to challenge these long standing assumptions. New tests (like the T2Lyme Panel by T2 biosystems) are utilizing the advances in PCR testing that accelerated due to the focus on COVID-19 testing during the pandemic.
T2 Biosystems are developing the T2Lyme Panel, a molecular diagnostic test designed to detect the bacteria Borrelia burgdorferi, which causes Lyme disease, directly from a blood sample. This test aims to improve early detection of Lyme disease by identifying the pathogen earlier than traditional antibody-based tests, which can take weeks to show a positive result.
T2 Biosystems plans to commercialize this test in the U.S. as a Laboratory Developed Test (LDT) and eventually pursue FDA clearance. Their innovation could significantly improve the accuracy and speed of Lyme disease diagnosis, particularly in the early stages when treatment is most effective (DETAILS HERE).
Emerging research also suggests that chronic Lyme disease may involve more complex mechanisms—including persistent infection or immune system dysfunction, which could explain why some patients do not respond to standard treatments. A review published in the Journal of Clinical Microbiology pointed to evidence of Borrelia burgdorferi, the bacterium responsible for Lyme disease, persisting in some patients despite antibiotic treatment. This finding has prompted calls for more nuanced research into the pathophysiology of chronic Lyme disease [5].
Recent Research and the Way Forward
A recent review of chronic Lyme disease research published in Infectious Disease Clinics of North America has highlighted the need for continued investigation into the long-term effects of Lyme disease and the potential for chronic infection. The review emphasized the importance of developing a standardized approach to diagnosing and treating chronic Lyme, based on the latest scientific evidence. This aligns with NASEM’s current study, which aims to provide clear guidance for clinicians and policymakers on how to manage this complex condition [4].
As NASEM’s study progresses, the medical community and policymakers are watching closely for its findings. The study is expected to deliver comprehensive recommendations on diagnosis, treatment, and patient care, which could lead to significant policy changes and improved outcomes for chronic Lyme patients. In parallel, other policy moves, such as increased federal funding for Lyme disease research and the development of new treatment guidelines by the CDC, are supporting this shift toward a more evidence-based approach to chronic Lyme disease [1].
This moment represents a critical juncture in the recognition and treatment of chronic Lyme disease—a condition that has long been marginalized but is now gaining the attention it deserves. With luck, by this coming spring, the outcomes of NASEM’s study will be available to guide the future of chronic Lyme disease management, offering hope to patients who have struggled for years to find answers and effective treatment.
Cited:
[1] NASEM, “Study on Lyme Infection-Associated Chronic Illnesses:” https://www.nationalacademies.org/our-work/the-evidence-base-for-lyme-infection-associated-chronic-illnesses-treatment
[2] CDC, “Lyme Disease Overview:” https://www.cdc.gov/lyme
[3] IDSA Guidelines: https://www.idsociety.org/practice-guideline/lyme-disease
[4] Infectious Disease Clinics of North America: https://www.id.theclinics.com/article/S0891-5520(21)00012-7/fulltext
[5] Journal of Clinical Microbiology: https://journals.asm.org/journal/jcm