Is There a Doctor in the House?
It’s a vicious cycle: Staffing shortages create increased workload for remaining staff, adding to burnout and exacerbating the shortages.
“The exhaustion I feel at the end of each shift is unlike anything I’ve experienced before COVID. It’s relentless.”
~Anonymous—American Medical Association Healthcare Workforce Burnout Survey
Healthcare workers across the U.S. have reached a breaking point as they contend with relentless patient demand, staffing shortages and personal mental health struggles. Consider the experiences above of a nurse in Boston who described her emotional state during the COVID-19 pandemic. Or the healthcare worker in an ICU in Arizona who was commenting on the overwhelming struggles the entire staff was facing.
The American Medical Association comments on an in-depth report on The Association of Work Overload with Burnout and Intent to Leave the Job Across the Healthcare Workforce During COVID-19 with a retrospective on some current suggestions on reducing burnout. It could be that a grassroots solution to personnel management can work or it may require a structural shift in the way health care is delivered. In either case, the sentiment that immediate action is required echoes across the country—from urban centers to rural communities—where shortages of staff have pushed many professionals beyond their limits.
“The constant influx of patients, combined with staff shortages, is wearing everyone down. I feel like I’m running on empty.”
~Anonymous—American Medical Association Healthcare Workforce Burnout Survey
The situation in Western Pennsylvania mirrors national trends, with local healthcare workers facing severe burnout and turnover rates. A 2022 University of Pittsburgh survey revealed that 73% of healthcare workers cited insufficient staffing as the primary reason for considering leaving their jobs. The pandemic only exacerbated these conditions, with healthcare professionals experiencing unprecedented levels of stress, burnout, and emotional exhaustion.
“We don’t get enough time to breathe between shifts, let alone deal with our mental health. We’ve been running on fumes for too long.”
~Anonymous—American Medical Association Healthcare Workforce Burnout Survey
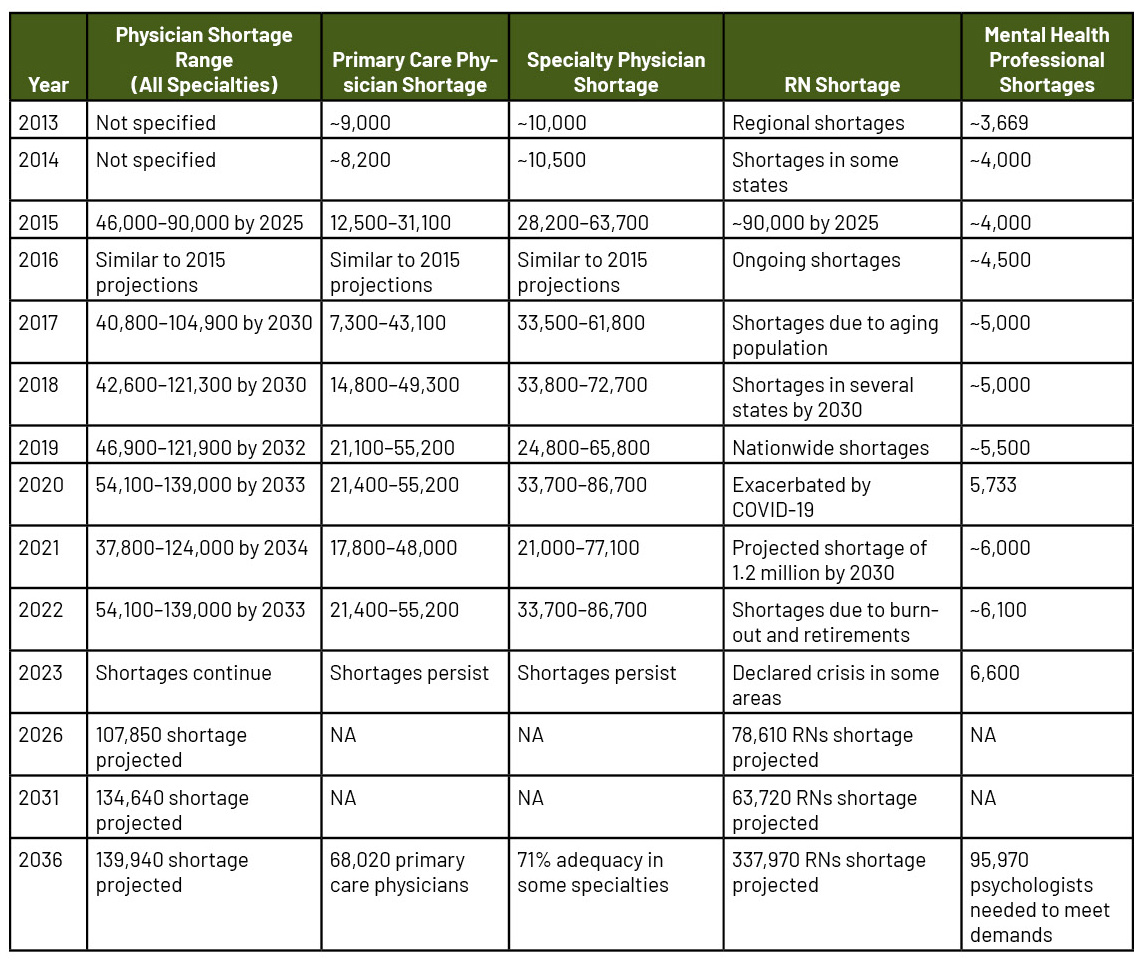
Staffing shortages have impacted various disciplines—from hospitals to long-term care facilities. The Pennsylvania Health Care Association (PHCA) projects a shortfall of 37,000 direct care workers by 2026, underscoring the urgency of addressing this crisis—scroll down to see chart below. Facilities offering retention bonuses and improved working conditions have reported modest improvements, but turnover remains high, especially in long-term care settings. For instance, nursing homes in Western Pennsylvania have struggled with maintaining adequate staffing levels, with turnover rates reaching unsustainable levels.
“You just don’t have time to decompress anymore. You go home exhausted, but then there’s another shift to prepare for. We’re losing good people who can’t take it anymore.”
~Anonymous—Biomed Central: “Global estimate of burnout among the public health workforce: a systematic review and meta-analysis”
Such stories resonate throughout the region, where nurses, aides and even administrative staff have reached their breaking point. The loss of healthcare professionals has begun to impact patient care, with facilities struggling to maintain continuity and quality of service.
Emotional and Physical Impact on Healthcare Workers
The emotional toll on healthcare workers has led many to leave the field altogether. According to a 2021 CIDRAP report, there was a 38% increase in healthcare workers leaving the industry, driven largely by burnout. A nurse who had been working for more than a decade explained, “I’ve been a nurse for 12 years, but the last two years during the pandemic were the hardest. It’s why I finally quit.”
The trend is creating a vicious cycle, as the remaining healthcare professionals face even greater workloads and stress—and is one reason why the impact of the COVID-19 pandemic on worker health has persisted. For many medical staff their workload only decreased as the patient headcount dropped. They may still be in emergency mode—at least as far as stress level goes.
The reality is that mental health has become a central issue in this crisis. Many workers feel isolated and unsupported by their organizations. One nurse in Western Pennsylvania shared her frustration:
“We’re expected to just deal with it—there’s no real support for our mental health. It feels like management just wants us to keep going until we break.”
~Anonymous—Biomed Central: “Global estimate of burnout among the public health workforce: a systematic review and meta-analysis”
Studies confirm that the lack of mental health resources for healthcare workers contributes significantly to burnout and turnover; the good news is that attempts are being made to address the situation.
One of the most recent and significant national programs addressing the mental health crisis among healthcare workers is the Impact Wellbeing™ Guide—developed by the CDC’s National Institute for Occupational Safety and Health (NIOSH) in collaboration with the Dr. Lorna Breen Heroes’ Foundation. Launched in 2024, this program specifically targets hospital leaders, providing them with evidence-based strategies to improve the professional wellbeing of healthcare workers.
The Impact Wellbeing Guide was pilot-tested in six hospitals, where it showed promising results in helping healthcare leaders address the burnout crisis by improving communication, reducing stigma around mental health and providing tools for long-term wellbeing.
Additionally, in 2022, the U.S. Congress passed the Dr. Lorna Breen Health Care Provider Protection Act, which allocates $35 million in grants to fund mental health programs for healthcare workers. This legislation focuses on reducing the stigma associated with seeking mental health care, offering more accessible services and providing educational resources to support healthcare professionals in managing stress and burnout.
In the Western Pennsylvania region, several local initiatives have been introduced to combat the healthcare staffing crisis and support workers’ mental health.
Allegheny Health Network (AHN) has taken a direct internal approach with its Resilience Training Program, launched in 2021. This program offers emotional regulation workshops, mindfulness sessions, and peer support groups to help clinical staff cope with the psychological strain of their roles.
“The workshops helped me develop coping mechanisms to deal with the stress. It’s not just about surviving each shift anymore.”
~Anonymous—Frontiers in Psychiatry: “Editorial: Practical interventions to tackle burnout in healthcare staff”
Since the program’s implementation, AHN has reported a 12% improvement in staff retention in high-stress areas like emergency departments, and a 10% increase in overall worker satisfaction. Wellness and retention programs for existing staff is important and shows how an organization values its assets. But organizations also need to hire more workers and provide the existing ones the tools to make them more efficient.
One of the most prominent staff training programs is UPMC’s Pathways to Work, which was launched in 2018. This initiative focuses on providing career advancement opportunities for entry-level healthcare workers.
“I started as a patient transporter, but through Pathways to Work, I’ve moved up into a more specialized role. It gives you a sense that there’s more to aim for.”
~Anonymous—Pathways to Work participant
The program has helped reduce turnover by 15% among support staff, offering them the chance to move into more specialized roles and avoid stagnation.
At the state level, the Pennsylvania Department of Health’s retention bonus program has provided immediate financial relief to overburdened staff, offering competitive wages and better working conditions. In facilities like at the Sunrise Nursing Home in Pittsburgh, these bonuses have resulted in a 20% reduction in turnover, with employees reporting improvements in their working conditions. However, as one healthcare worker pointed out, “Bonuses are nice, but they don’t fix the fact that we’re understaffed every single day.” While bonuses have provided temporary relief, systemic reforms are still needed to address long-term workforce challenges.
National Comparisons and Broader Implications
Other states have also adopted various approaches to combat turnover. For instance, Massachusetts expanded its nursing education pipeline by offering tuition reimbursements and fast-track certification programs, resulting in an 8% reduction in turnover rates.
“The fast-track certification program allowed me to get my degree quicker and start working. It helped me feel more confident about my career.”
~Anonymous—MASSGrant Plus Expansion Program participant
Programs like MASSGrant Plus cover the full cost of tuition for eligible students, providing additional financial relief to future healthcare workers, ensuring that the nursing pipeline remains robust and capable of meeting healthcare demands.
Some progress has been made—particularly with programs like UPMC’s Pathways to Work and AHN’s Resilience Training—but the system still struggles to address the underlying causes of burnout and turnover. Many healthcare professionals remain overworked, underpaid and mentally exhausted. Short-term solutions like retention bonuses and career advancement programs have helped to some extent, but they are insufficient to address the broader issues driving burnout and turnover. Without significant changes to staffing levels, mental health support, and leadership engagement, the crisis is likely to persist.
The challenges facing our healthcare staff and the system that they enable are not trivial, but they are also being acknowledged—which provides hope. The 2023 State of Healthcare Performance Improvement Report also highlighted that, while staffing challenges persist, there is a decrease in the utilization of contract labor in many organizations. This signals some stabilization in staffing levels as hospitals and health systems slowly climb back toward more sustainable operating conditions.
Watch this space for further articles on Healthcare Worker Satisfaction and efforts to improve efficiency and effectiveness of care delivery. If policy changes can’t solve the problem perhaps innovation can.